Key Takeaways
Structured Documentation SOAP notes provide a standardised four-part framework for consistent clinical record-keeping across all healthcare settings.
Legal Protection Comprehensive SOAP documentation serves as crucial evidence for clinical decision-making and provides medico-legal protection.
Continuity of Care SOAP notes ensure seamless communication between healthcare providers and maintain treatment consistency over time.
Quality Improvement Regular SOAP note review enables clinical audit, quality assurance, and evidence-based practice refinement.
What is a SOAP Note?
A SOAP note represents the gold standard in clinical documentation, providing healthcare professionals with a methodical approach to recording patient encounters. This internationally recognised format ensures that every aspect of a patient consultation is captured systematically, from initial presentation through to treatment planning.
The SOAP methodology divides clinical documentation into four distinct sections. The Subjective component captures the patient's own account of their symptoms, concerns, and medical history as they describe it. However, the Objective section documents measurable clinical findings, including vital signs, physical examination results, and diagnostic test outcomes.
Furthermore, the Assessment section demonstrates the clinician's professional analysis, where differential diagnoses are considered and clinical reasoning is documented. Finally, the Plan section outlines the proposed course of action, including treatments, referrals, follow-up appointments, and patient education requirements.
How to use SOAP Note?
Step 1: Download SOAP Note Template
First, access the SOAP note PDF document by downloading it from Pabau below. The template provides pre-formatted sections that guide you through each component of the documentation process, ensuring nothing is overlooked during patient encounters.
Step 2: Complete the Subjective Section
Begin by documenting the patient's chief complaint in their own words, followed by their description of symptoms, pain levels, and any relevant medical history. Include information about current medications, allergies, and social factors that may impact their condition.
Step 3: Record Objective Findings
Document all measurable and observable data, including vital signs, physical examination findings, laboratory results, and imaging studies. Record specific measurements, test scores, and clinical observations using precise medical terminology.
Step 4: Develop Your Assessment
Analyse the subjective and objective information to formulate your clinical impression. List differential diagnoses in order of likelihood and provide your rationale for each diagnostic consideration based on the available evidence.
Step 5: Create the Treatment Plan
Outline your proposed interventions, including immediate treatments, prescribed medications, lifestyle modifications, and referrals to other healthcare professionals. Include specific follow-up instructions and patient education requirements.
Step 6: Review and Finalise
Ensure all sections are complete, accurate, and legible. Verify that your documentation supports your clinical decisions and provides sufficient detail for continuity of care should another provider need to review the case.
Who is it helpful for?
SOAP notes serve as an invaluable tool for healthcare professionals across diverse clinical settings. General practitioners benefit from the structured approach when managing complex patients with multiple comorbidities, as the format ensures comprehensive assessment and systematic treatment planning.
Specialists in fields such as physiotherapy, chiropractic care, and sports medicine find SOAP notes particularly beneficial for tracking patient progress over multiple sessions. The format allows these practitioners to monitor treatment effectiveness and adjust therapeutic interventions based on documented outcomes.
In addition, mental health professionals including psychologists and counsellors utilise SOAP notes to document therapeutic sessions, track patient progress, and maintain detailed records of treatment modalities employed. The structure supports both individual therapy documentation and multidisciplinary team communication.
Benefits of using SOAP Note
- Standardised documentation format recognised across all healthcare disciplines
- Enhanced communication between healthcare team members and specialists
- Improved clinical decision-making through systematic information organisation
- Strong medico-legal protection through comprehensive record-keeping
- Streamlined billing and coding processes for insurance purposes
Regular implementation of SOAP note documentation significantly enhances clinical practice quality whilst ensuring regulatory compliance. This systematic approach reduces the risk of important clinical information being overlooked, ultimately leading to improved patient outcomes and professional accountability in healthcare delivery.
Quality Assurance in Clinical Documentation
SOAP note implementation supports robust quality assurance programmes within healthcare organisations. Regular review of SOAP documentation enables clinical supervisors to assess practitioner competency, identify areas for improvement, and ensure adherence to clinical guidelines. This systematic approach to documentation review facilitates peer learning and maintains high standards of patient care across the organisation.
Moreover, the structured nature of SOAP notes makes them invaluable for clinical audit purposes. Healthcare organisations can analyse patterns in diagnosis, treatment approaches, and patient outcomes, leading to evidence-based improvements in clinical protocols and patient care pathways.
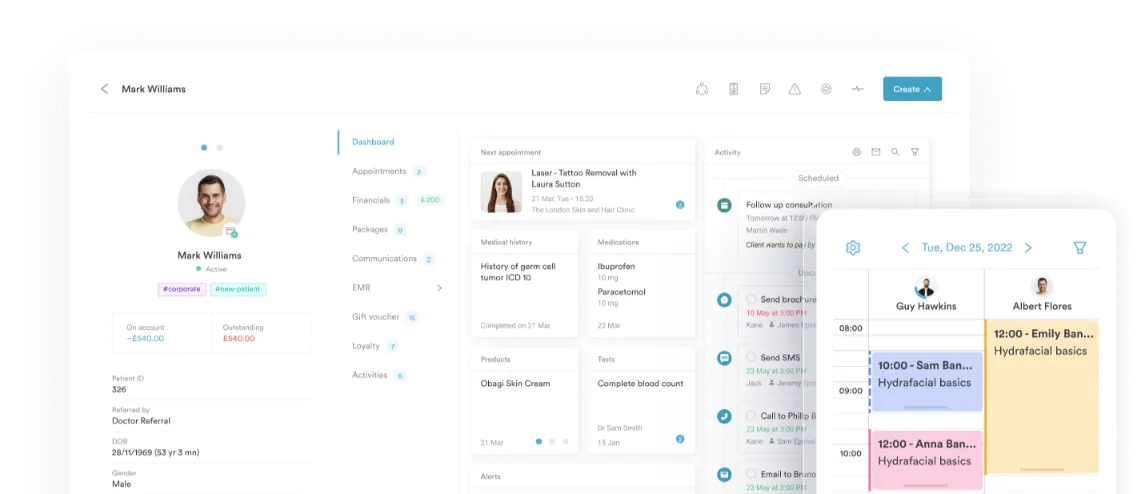
Integration with Electronic Health Records
Modern SOAP note templates integrate seamlessly with electronic health record systems, enhancing efficiency whilst maintaining documentation quality. Digital SOAP formats often include drop-down menus, standardised terminology, and automatic calculation features that reduce documentation time whilst improving accuracy.
Furthermore, electronic SOAP notes facilitate real-time access to patient information across multidisciplinary teams. This immediate availability of comprehensive clinical data supports coordinated care delivery and reduces the risk of communication gaps between different healthcare providers involved in a patient's treatment journey.
SOAP Note